I have been struggling to sleep the last several weeks. I fall asleep fine – generally tired out by the events of the day, but I wake up a few times each night and then drag myself out of bed at 5 AM to start the day. I notice I am not as patient as I could be and not as kind. That’s not usual for me. I think it’s because of recent and ongoing events – the war in Israel, the humanitarian crisis in Gaza, the mass shooting in Maine, the lack of civil discourse in the country and world… to name just a few of the many things on my mind. It makes me scared for the future, and sometimes leaves me feeling paralyzed as to what I can do, if anything, to be of help.
This is hard and takes a toll. And so, I thought I would reach out to a friend and colleague, Dr. Jessica Gold, an Assistant Professor in the Department of Psychiatry who specializes in the mental health of healthcare workers, women and students, and who speaks broadly on these topics to get some advice for me that I hope will be helpful for the rest of you.
As healthcare workers, we routinely experience challenging things – death, trauma, violence. It feels normal to be affected by it. When do we need to be worried that we need to seek help for ourselves?
I think it is as normal to be affected by it as to not be affected by it, and both responses warrant us to pay some attention.
To those of us who have something difficult happen and then we grieve, we feel, we lose sleep, but then it eases over time, or doesn’t interfere with our lives, that is normal. We are allowed to feel things about our jobs and the world because both are difficult and hard and that’s OK. We should normalize that response and not pathologize it. It’s when those feelings start to interfere with our lives and day-to-day activities (not just work, think socializing too), that we should be more concerned. Or, if it lasts longer or worsens. Then, we should consider asking for help, which is not a weakness, but a strength.
To those of us who learned to cope by not feeling, know that numbness is a feeling too. Medicine often teaches us to disconnect from a trauma at work to go to the next case, and there is a bit of safety in that response, honestly, but know that only works for so long. Kind of like a beach ball in the water, it eventually comes back up in full force. We need to pay attention to not feeling, too, and how it can interfere with our lives and our functioning, just as much as feeling, and if it does, we should ask for help. I wrote some about that here.
When there is a regional, national, or international crisis that is affecting us personally, what are some strategies we can use to cope?
I am a big believer in the fact that the strategy that works in these situations is that strategy that you will use. I could rattle off a list of coping skills that work for people – meditation, journaling, exercise, socializing, deep breathing – but honestly what works is what you will do and use and find helpful. I usually tell people to try out some things, and not beat yourself up if you don’t love the one everyone else seems to love. I am a big fan of all the tools Duke has here, because they are short and made for people in healthcare. I also personally tend to turn to a combination of mindless television, therapy, my dog, and journaling, if that helps.
Other important things to do are actually checking in on yourself and making time for that. We spend so much time checking in on others, and often throw ourselves even further into that when the world is hard and helping people at work makes us feel good, but we need to check on ourselves, too. Self-compassion in these circumstances comes in handy, especially because the world adds a lot of weight. Try to hear that voice in your head tell you “I am worthless” when you make a mistake, and try to reframe that in a way you would speak to a friend instead, “mistakes are normal, don’t beat yourself up about it, maybe there’s something to learn from it instead.”
On top of all of that, having someone you can turn to – a supportive friend, coworker, or supervisor, can make a huge difference and is protective often against things like burnout and depression. Ask someone else how they are doing, and actually mean it.
In this newsletter, I am including an article by a respected epidemiologist who talked about the trauma that can be caused by watching too much news, or engaging too much in social media in the midst of such crises. Thoughts on this?
I have a lot of thoughts on this, and it reminds me of a cartoon in the New Yorker from some time in 2020.
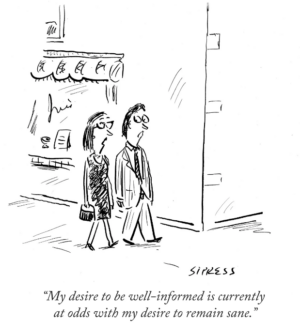
I think that sums up how I have felt for years about the intersection between social/news and mental health, and how most of my patients feel, but as an avid social media user/news consumer myself, I will say the best thing you can do for yourself is mindfully consume it. I would never tell someone the answer is to never use it, or to not stay informed, because at least in my line of work it is nearly impossible to do that as the world affects why someone is in my office. But, I will say, if you notice yourself not sleeping and staying up to scroll, or grinding your teeth while looking, or getting sad, or angry, those are all cues that you probably need at least a break, as you can absolutely be affected by more time on it, and what you are seeing. I try to pay attention to my body and emotions, and make adjustments accordingly, and really try not to look at things the 30 minutes to 1 hour before bed, even if that means my phone can’t be my alarm clock (turns out they still make real ones). I will also say that during hard times, there is an urge to post on social, and sometimes you need to pause there, too. That is OK and no one should make you feel bad for that.
I have some basic strategies that help me in times of stress – regular exercise, good sleep habits, and a gratitude practice. When the world around me feels out of control, I feel like these kinds of things are even more important but also may not be enough. In those times, I have found that intentional outreach to friends, family, and being present in and noticing the beauty of certain rituals and traditions (White Coat Ceremony, pumpkin carving, the changes in the leaves and light as fall descends) really help. Am I just making this up, or is there value to these strategies? What else can work?
All of these strategies are important and logical and I, for one, am grateful for you sharing. Things like anxiety don’t like when things are out of control (loss of control is kind of the enemy of anxiety), so finding even subtle ways to regain some of it like exercise or sleep, can make a huge difference. Gratitude has a lot of evidence, and even if people want to tell me it seems cheesy, I try to tell them the point is not to ignore the bad, it is to notice the good. In other words, we are often so bogged down by all the bad that we fail to remember that anything good happens. Trying to make ourselves remember is not toxic positivity – it is just balance – kind of like noticing the beauty in rituals.
Again, overall, I stick with my feeling that what works is what you do, and we should treat coping like a hobby. There are these lists of pleasant activities that can sometimes be a place to start if you can’t think of anything you might like, and sometimes other people’s words or images through poetry, memes, song lyrics, or art can help us find how we feel. Also, therapy is not only for times of acute distress. Sometimes it just helps to have an external person to talk and process with, and there is no harm in wanting that.
Any last words of wisdom?
Anything you are feeling is normal and feelings themselves are not something to beat yourselves up about. There are no good or bad feelings (e.g. I am a big fan of anger and what it tells you), and as it turns out, we can be good at our jobs, and have feelings/be human….who knew.
I want to thank Dr. Gold for these wise words.
So, what are my (Eva’s) take home points? We are living in a complex and challenging time. As healthcare professionals and learners, and the people who train and support them, we are particularly prone to caring deeply about others (thank goodness!) and being impacted by what is going on in the world. This also impacts our patients. We need to be aware of when we are not doing ok and seek help. We can do some things to protect ourselves, ground ourselves in the things that give us meaning and purpose, and pay intentional attention to the small, beautiful things that happen every day and every season or year. And we need to be a part of the change that supports civil discourse, respect, kindness and grace, through our actions and teachings. Every day.
If you or someone you know need help, please reach out.
Options for faculty, housestaff and staff.