What I love about sports is that for a team to succeed, each team member must know their role and responsibility even in individual sports like tennis – trainers, coaches, racquet stringers.
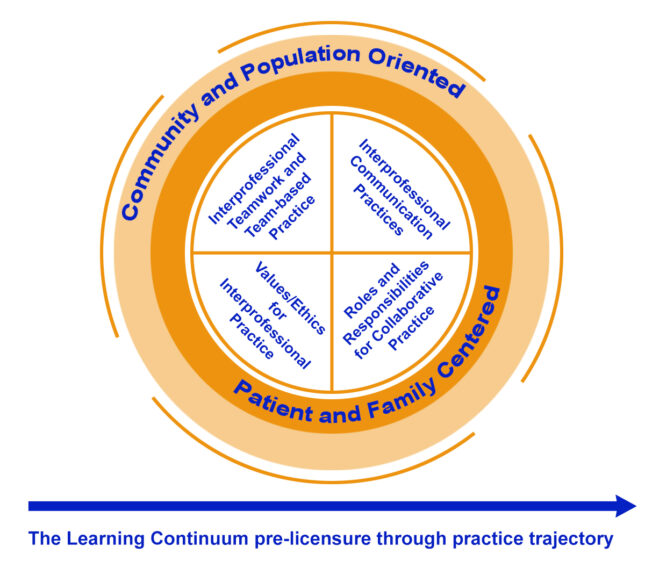
Just like athletes, future physicians must learn to work effectively on healthcare teams which are complex and require the cooperation of many different health professionals. In the Gateway curriculum, our approach to interprofessional education (IPE) began with a review of the 4 Competency Domains created by the Interprofessional Education Collaborative (IPEC), a collaboration of 21 national health professional associations (https://www.ipecollaborative.org/membership): Interprofessional Communication, Roles and Responsibilities, Values and Ethics and Interprofessional Teamwork. These competencies are meant to be achieved over a lifetime from training to practice.
With these IPEC competencies and our guiding light of finding “natural fits” where IPE could be highlighted in mind, we began in phase 1 by collaborating with Module leads to integrate the roles and responsibilities of our interprofessional colleagues within what they were already teaching. This ranged from having social workers on panels talking about organ transplant to having physical therapy senior students teaching musculoskeletal exams to Phase 1 Gateway students through clinical vignettes. In this way, phase 1 students saw the expertise our interprofessional colleagues possess and the vital role they play in patient care.
We also focused on integrating interprofessional communication and teamwork. The Center for Interprofessional Practice and Education (CIPE) already coordinated sessions with early learners from all schools on the Washington University Medical Campus (Audiology, Genetics, Medicine, Nursing, Occupational Therapy, Pharmacy, Physical Therapy) to learn about social and structural determinants of health, and interprofessional communication and teamwork. We deliberately integrated what was learned in the CIPE sessions into the Gateway curriculum around communication and health, equity and justice (HEJ) – often highlighting the interprofessional perspective. For example in the HEJ curriculum, we had occupational therapy (OT) faculty and an OT doctorate student teach about housing insecurity and the role OT plays in working with the unhoused here in St Louis.
We further took advantage of the clinical immersions in Phase 1 of the Gateway Curriculum, where phase 1 students are placed on healthcare teams for 3 weeks at a time with no classroom responsibilities. This was a unique opportunity for the students to see and meet first hand our interprofessional colleagues that they had learned about in the Modules. Immersion students were required to interview and shadow at least 1 non-MD health professional working with their clinical team whether that was a nurse, physical therapist, coder, biller or social worker. Through this activity, Gateway students gained a better understanding of the challenges and responsibilities each member of the healthcare team faces. They are then required to incorporate this into their end of immersion analysis on healthcare teams.
Now in Phase 2, the Gateway students are immersed in their clerkships and we are pushing them to further incorporate interprofessional roles and responsibilities, teamwork and communication into their emerging role as a physician. Students on the Neurology clerkship are placed in physician clinics that have interprofessional practitioners integrated into the work flow and also placed them in non-physician centered clinics such as a stroke occupational therapy clinic or the Stephen A. Orthwein Center at Paraquad which is a fully accessible gym for people with disabilities staffed solely by occupational and physical therapy practitioners.
Phase 2 students are also asked to incorporate their interprofessional skills into their decision making. In one of our standardized patient team scenarios, students create a discharge plan for a stroke patient alongside other interprofessional students and receive feedback on their teamwork and communication skills. Moreover, students are required to turn in physician notes that focus on interprofessional team members that should be included in a patient’s care based on the specific needs of the patient and healthcare team and, importantly, how interprofessional teams caring for patients support high value patient care.
As we finalize our phase 3 curriculum, we hope to continue to find “natural fits” for our students to further their skills around Interprofessional Communication, Roles and Responsibilities, and Interprofessional Teamwork. And since phase 3 Gateway students will have spent significant time in clinical areas, we will have phase 3 students begin to explore the Values and Ethics around interprofessional collaboration.
Hopefully at graduation, our Gateway students will have a great base of skills and habits that will help them succeed on interprofessional health care teams as trainees and as physicians and continue their life long journey of interprofessional education and collaboration.